The Most Up To Date Guidelines, At Your Fingertips
CCS Pocket Guides
-
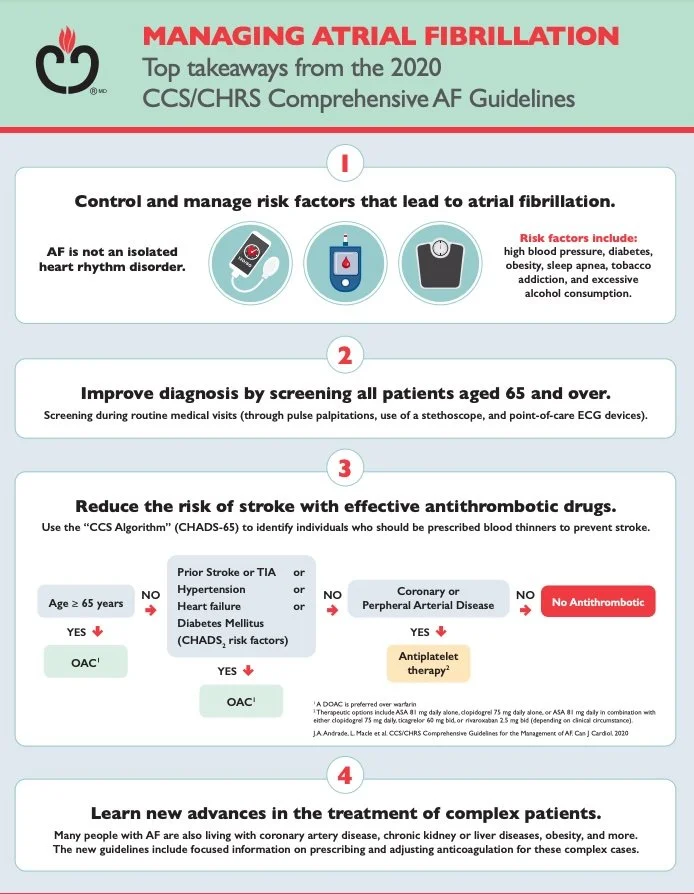
1. AF Classification
Paroxysmal AF: Self-terminating (≤7 days).
Persistent AF: Sustained >7 days or requiring cardioversion.
Long-standing Persistent AF: Continuous >12 months.
Permanent AF: Accepted by patient/physician (no further attempts to restore sinus rhythm).
2. Stroke Risk Assessment (CHADS-65)
CHADS-65 Score:
Congestive heart failure (1 point)
Hypertension (1)
Age ≥65 (1)
Diabetes (1)
Stroke/TIA/systemic embolism (2 points)
Anticoagulation:
DOACs first-line (apixaban, rivaroxaban, dabigatran, edoxaban) for CHADS-65 ≥1 (men) or ≥2 (women).
Avoid in severe renal impairment (use warfarin).
Consider LAA occlusion (e.g., Watchman) if anticoagulation contraindicated.
3. Rate vs. Rhythm Control
Rate Control:
First-line: Beta-blockers (e.g., metoprolol) or non-DHP CCBs (diltiazem/verapamil).
Digoxin: Reserved for sedentary patients or HFrEF.
Rhythm Control:
Antiarrhythmics:
No structural heart disease: Flecainide, propafenone.
HF or CAD: Amiodarone, sotalol.
Catheter Ablation: Recommended earlier (e.g., symptomatic paroxysmal/persistent AF refractory to meds).
4. Acute AF Management
Hemodynamically Unstable: Immediate cardioversion.
Stable Patients:
Rate control: IV metoprolol/diltiazem.
Rhythm control: Electrical or pharmacological cardioversion (e.g., ibutilide) if onset <48h (or confirmed no thrombus).
Anticoagulation: Start immediately (unless contraindicated).
5. Integrated Care (ABC Pathway)
Anticoagulation to prevent stroke.
Better symptom management (rate/rhythm control).
Cardiovascular risk and comorbidity management (e.g., HTN, OSA, obesity).
6. Lifestyle & Comorbidities
Weight loss: Reduces AF burden in obese patients.
Alcohol: Limit to ≤2 drinks/day.
Exercise: Moderate aerobic activity (avoid excessive endurance training).
Screen for OSA: Especially in resistant AF.
Key Updates (2021)
DOACs preferred over warfarin in most cases.
Earlier referral for ablation (Class I recommendation for symptomatic AF).
CHADS-65 replaces CHA₂DS₂-VASc for simplicity.
Focus on lifestyle modifications (weight loss, alcohol reduction).
Clinical Pearl: Use the 4S-AF scheme to guide management:
Stroke risk (anticoagulate) → Symptoms (rate/rhythm control) → Severity (comorbidities) → Substrate (lifestyle).
-
1. Classification
HFrEF: EF ≤40% (reduced ejection fraction).
HFmrEF: EF 41–49% (mid-range).
HFpEF: EF ≥50% (preserved).
2. Diagnosis
Symptoms/Signs: Dyspnea, fatigue, orthopnea, edema, elevated JVP, rales.
Key Tests:
BNP/NT-proBNP: Elevated levels (BNP >35 pg/mL; NT-proBNP >125 pg/mL) support HF diagnosis.
Echo: Mandatory for EF assessment and structural evaluation (e.g., valve disease, wall motion abnormalities).
ECG/CXR/Labs: Rule out ischemia, arrhythmia, pulmonary edema, anemia, renal dysfunction.
3. Chronic Management
A. HFrEF(Core Therapies)
First-line:
ARNI (sacubitril/valsartan) or ACEi/ARB.
Beta-blockers (bisoprolol, carvedilol, metoprolol).
MRA (spironolactone/eplerenone).
Add-ons:
SGLT2i (dapagliflozin/empagliflozin) – now recommended for all HF subtypes.
Ivabradine: If HR >70 bpm on beta-blocker.
Diuretics (e.g., furosemide) for volume overload.
Devices:
ICD: Primary prevention if EF ≤35% despite 3+ months of GDMT.
CRT: For QRS >150 ms (LVEF ≤35%).
B. HFmrEF/HFpEF:
Manage comorbidities (HTN, AF, diabetes, obesity).
Empagliflozin reduces hospitalizations in HFpEF.
Diuretics for symptomatic relief.
4. Acute Decompensated HF
Identify Triggers: Infection, non-compliance, ischemia, arrhythmia.
Therapy:
IV loop diuretics (e.g., furosemide) for congestion.
Vasodilators (nitroglycerin) if BP >110 mmHg.
Inotropes (dobutamine) or vasopressors (norepinephrine) in cardiogenic shock.
Monitor electrolytes, renal function, and volume status.
5. Lifestyle & Prevention
Patient Education: Sodium/fluid restriction, daily weight monitoring.
Exercise: Cardiac rehab improves outcomes.
Vaccinations: Influenza/pneumococcal.
Key 2021 Updates
SGLT2i expanded to all HF subtypes (reduces mortality/hospitalization).
ARNI preferred over ACEi/ARB in HFrEF.
Empagliflozin now indicated for HFpEF.
Clinical Pearl: Start GDMT early in HFrEF (titrate rapidly!) and prioritize SGLT2i as a foundational therapy.
-
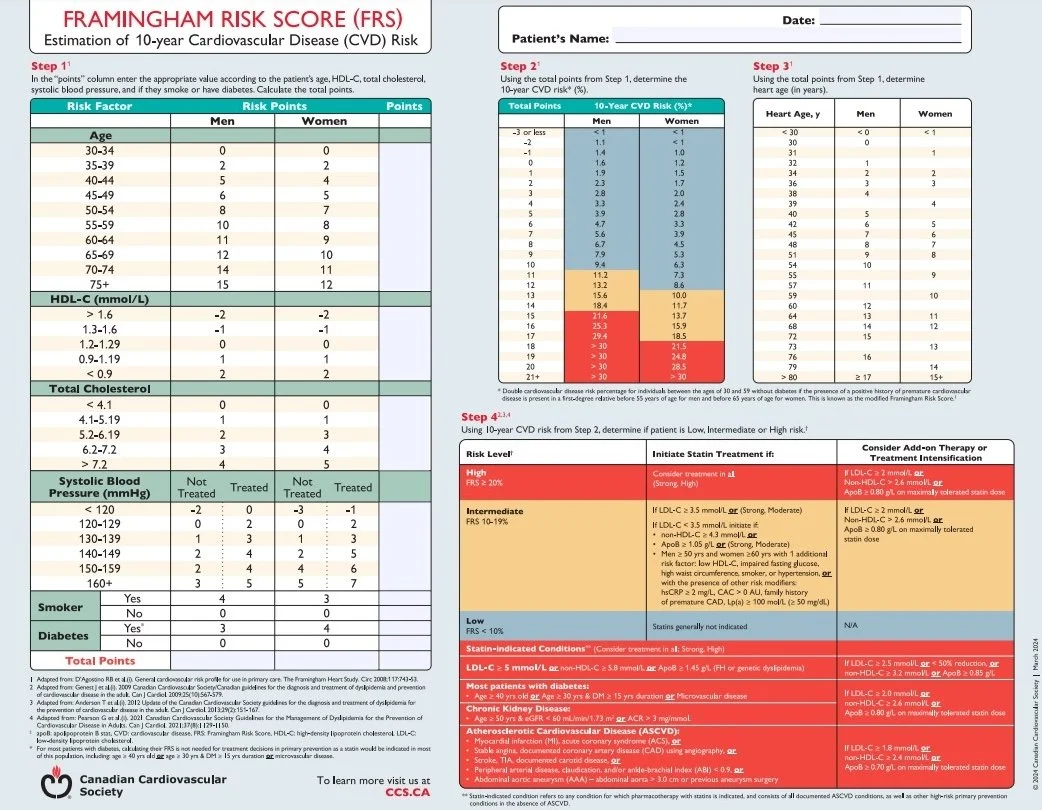
1. Risk Stratification
Prioritize ASCVD risk:
Very High Risk: Clinical ASCVD (e.g., CAD, stroke, PAD) or diabetes with end-organ damage.
High Risk: Diabetes ≥40 years, CKD (eGFR <60), or FRS ≥20%.
Moderate Risk: FRS 10-19%.
Low Risk: FRS <10%.
2. LDL-C Targets
Very High Risk: <1.8 mmol/L (or ≥50% reduction from baseline).
High Risk: <2.0 mmol/L (or ≥50% reduction).
Moderate/Low Risk: <3.4 mmol/L.
3. First-Line Therapy
High-Intensity Statins:
Atorvastatin 40-80 mg or rosuvastatin 20-40 mg for very high/high risk.
Moderate-intensity statins for lower-risk patients.
Combination Therapy (if targets not met):
Add ezetimibe (reduces LDL-C by ~20%).
PCSK9 inhibitors (alirocumab, evolocumab) for very high-risk patients failing statin + ezetimibe.
4. Hypertriglyceridemia
Triglycerides ≥5.6 mmol/L:
Rule out secondary causes (alcohol, diabetes, hypothyroidism).
Fibrates (e.g., fenofibrate) or omega-3 fatty acids (icosapent ethyl 4 g/day) to reduce pancreatitis risk.
5. Special Populations
Diabetes:
LDL-C target <2.0 mmol/L if ≥40 years or with microvascular complications.
Familial Hypercholesterolemia (FH):
Screen family members; treat aggressively with statins + ezetimibe ± PCSK9 inhibitors.
6. Monitoring & Safety
Baseline: Check lipids, LFTs, CK.
Follow-up: Repeat lipids at 3 months; monitor for statin side effects (myalgias, elevated LFTs).
Safety: Avoid statins in pregnancy; use caution in CKD.
7. Lifestyle Interventions
Diet: Mediterranean diet, minimize saturated/trans fats.
Exercise: ≥150 min/week moderate-intensity activity.
Smoking cessation: Critical for ASCVD risk reduction.
Key 2022 Updates
Lower LDL-C targets for very high-risk patients (<1.8 mmol/L).
Icosapent ethyl recommended for ASCVD patients with persistent TG ≥1.5 mmol/L despite statins.
Inclisiran (small interfering RNA therapy) now approved as adjunct for FH/ASCVD.
Emphasis on lifetime risk: Earlier intervention in younger patients with FH or high genetic risk.
Clinical Pearl: Start high-intensity statins early in high/very high-risk patients; treat to target and escalate therapy aggressively if needed.
-
1. Primary Prevention
Routine aspirin not recommended for asymptomatic adults without CVD.
Exceptions: Consider in select high-risk diabetes patients (40–70 years) after individualized risk-benefit discussion.
2. Secondary Prevention in Stable CAD
Lifelong low-dose aspirin (75–100 mg/day).
Dual antiplatelet therapy (DAPT) not routinely recommended unless recent ACS or PCI.
3. Acute Coronary Syndrome (ACS)
DAPT for 12 months:
Aspirin + potent P2Y12 inhibitor (ticagrelor or prasugrel preferred over clopidogrel).
Exceptions:
Prasugrel contraindicated in prior stroke/TIA or age ≥75.
Clopidogrel if ticagrelor/prasugrel not tolerated.
Early de-escalation (e.g., switching to clopidogrel) may be considered in high bleeding risk.
4. Post-Percutaneous Coronary Intervention (PCI)
DAPT Duration:
ACS patients: 12 months (minimum 6 months if high bleeding risk).
Elective PCI: 1–6 months based on stent type (BMS vs. DES) and bleeding risk.
Extended DAPT (>12 months): Consider in high ischemic/low bleeding risk (e.g., complex PCI, prior MI).
5. Atrial Fibrillation + CAD (Triple Therapy)
Combining antiplatelets + anticoagulants:
Short-term triple therapy (aspirin + clopidogrel + DOAC) for 1–6 weeks post-PCI/ACS.
Transition to dual therapy (clopidogrel + DOAC) for up to 12 months.
Use CHA2DS2-VASc and HAS-BLED scores to guide decisions.
6. Special Populations
CABG: Resume DAPT post-surgery if ACS indication.
High Bleeding Risk:
Shorten DAPT duration (e.g., 3–6 months).
Use proton pump inhibitors (PPIs) with DAPT to reduce GI bleeding.
Renal Impairment: Avoid prasugrel; prefer clopidogrel or ticagrelor.
7. Perioperative Management
Elective surgery: Stop P2Y12 inhibitors 5–7 days pre-op (if possible).
Aspirin: Continue perioperatively unless high bleeding risk.
8. Key Updates (2018)
Personalized DAPT duration: Tailor to ischemic/bleeding risk (e.g., PRECISE-DAPT or DAPT score).
De-escalation strategies: Transition from potent P2Y12 inhibitors to clopidogrel in high bleeding risk.
Ticagrelor/prasugrel preferred over clopidogrel in ACS.
Clopidogrel monotherapy may replace aspirin in aspirin-intolerant patients.
Clinical Pearl: Balance ischemic vs. bleeding risk in every patient. When in doubt, default to 12 months DAPT for ACS/PCI, but shorten duration in high bleeding risk.
-
1. Definition & Classification
Cardiorenal Syndrome (CRS): Bidirectional dysfunction of the heart and kidneys, classified into 5 types:
Type 1: Acute cardiac dysfunction → acute kidney injury (e.g., ADHF).
Type 2: Chronic cardiac dysfunction → progressive CKD (e.g., chronic HFrEF).
Type 3: Acute kidney injury → acute cardiac dysfunction (e.g., volume overload).
Type 4: Chronic CKD → chronic cardiac disease (e.g., LVH, HFpEF).
Type 5: Systemic disease (e.g., sepsis, diabetes) → simultaneous cardiac/kidney injury.
2. Diagnostic Workup
Cardiac Assessment:
BNP/NT-proBNP (elevated in HF).
Echocardiography (LVEF, diastolic function, valvular disease).
Renal Assessment:
Serum creatinine/eGFR, urine albumin-to-creatinine ratio (ACR).
Renal ultrasound (rule out obstruction).
Rule Out: Hypovolemia, nephrotoxins (NSAIDs, contrast), sepsis.
3. Management Principles
A. Heart Failure with CRS
GDMT for HFrEF:
ARNI/ACEi/ARB, beta-blockers, MRAs, SGLT2 inhibitors (e.g., dapagliflozin, empagliflozin).
Adjust doses for eGFR (e.g., avoid ARNI if eGFR <30).
Diuretics:
Loop diuretics (furosemide) for volume overload; combine with thiazides if refractory.
Monitor electrolytes (K+, Mg²⁺).
B. Kidney Protection
ACEi/ARBs or SGLT2 inhibitors for proteinuria.
Avoid nephrotoxic agents (NSAIDs, iodinated contrast).
Referral: Nephrology consult if eGFR <30 or rapid decline.
C. Advanced Therapies
Ultrafiltration: Consider in diuretic-resistant volume overload.
Dialysis: For refractory hyperkalemia, acidosis, or uremia.
4. Special Considerations
Hyperkalemia:
Use patiromer or sodium zirconium cyclosilicate if chronic.
Limit ACEi/ARB/MRA doses if recurrent.
Anemia: Treat iron deficiency (IV iron preferred in CKD).
Palliative Care: For end-stage CRS with poor prognosis.
5. Key 2023 Updates
SGLT2 inhibitors recommended for all CRS types (reduce HF hospitalizations and CKD progression).
ARNI preferred over ACEi/ARB in HFrEF with CKD (better renal outcomes).
Individualized diuretic regimens (avoid over-diuresis worsening renal function).
Biomarkers: Emerging role of galectin-3 and sST2 for risk stratification.
6. Lifestyle & Monitoring
Sodium/fluid restriction: ≤2–3 g/day Na⁺; daily weights.
Diet: Low-protein diet in advanced CKD (individualized).
Monitoring:
Weekly labs (creatinine, K⁺) during GDMT titration.
eGFR trajectory (decline >30% warrants reassessment).
Clinical Pearl: Prioritize SGLT2 inhibitors (cardio-renal-metabolic benefits) and multidisciplinary care (cardiology/nephrology collaboration).
-
1. Indications for CRT
Primary Candidates:
Sinus rhythm, LVEF ≤35%, NYHA class III/IV (or ambulatory class IV) on optimal medical therapy, with:
LBBB morphology + QRS duration ≥150 ms (Class I recommendation).
LBBB + QRS 120–149 ms (Class IIa).
Non-LBBB + QRS ≥150 ms (Class IIb).
Milder Symptoms (NYHA II):
LVEF ≤30%, LBBB + QRS ≥150 ms, ischemic cardiomyopathy (Class I).
2. Device Selection
CRT-P (Pacemaker): For symptom relief and LV reverse remodeling.
CRT-D (Defibrillator): Add defibrillator function if life-threatening arrhythmia risk (e.g., prior sudden cardiac arrest, ischemic cardiomyopathy).
3. Implantation Procedure
LV Lead Placement: Target lateral/posterolateral coronary vein for optimal resynchronization.
Coronary Sinus Venography: Essential for anatomical mapping.
Device Programming: Optimize AV/VV intervals (echocardiography-guided).
4. Follow-Up & Optimization
Post-Implant:
Assess pacing thresholds, lead stability, and phrenic nerve stimulation.
Repeat echocardiography at 3–6 months to evaluate LVEF improvement.
Non-Responders (~30% of patients):
Verify >95% biventricular pacing.
Optimize medical therapy (diuretics, neurohormonal agents).
5. Contraindications
Mechanical right heart valve.
Expected survival <1 year.
Permanent atrial fibrillation without pacemaker control (unless AV nodal ablation planned).
6. Special Populations
Atrial Fibrillation:
CRT may still benefit if ventricular rate controlled (e.g., AV nodal ablation + CRT).
Right Bundle Branch Block (RBBB): Limited benefit; consider only if QRS ≥150 ms + LVEF ≤35%.
7. Outcomes
Reduced Mortality/Hospitalizations: Supported by trials (e.g., COMPANION, CARE-HF).
Symptom Improvement: 60–70% patients show better functional class, quality of life.
Key 2013 Updates
Expanded indications for NYHA class II patients with wide QRS/LBBB.
Emphasis on LBBB morphology as a predictor of CRT response.
Refined ECG criteria (QRS duration + morphology).
Clinical Pearls:
Prioritize LBBB + QRS ≥150 ms for maximal benefit.
Ensure >95% biventricular pacing; address AF or frequent PVCs that reduce pacing efficacy.
Multidisciplinary care (HF specialist, electrophysiologist) improves outcomes.
-
1. Diagnosis & Risk Stratification
Clinical Evaluation:
Symptoms: Assess for classic angina (retrosternal discomfort, exertion/emotional triggers) and nonclassical presentations (e.g., in diabetes).
Risk Factors: Modifiable (smoking, dyslipidemia, diabetes) and nonmodifiable (age, family history).
Tests: ECG, lipid panel, fasting glucose, renal/hepatic/thyroid function, hemoglobin A1c.
Pretest Probability: Use age, sex, and symptom characteristics to guide testing. Avoid testing if pretest probability is <10% or >90%.
Noninvasive Testing:
Exercise ECG: First-line if interpretable and patient can exercise.
Imaging (SPECT, echocardiography, CCTA): For uninterpretable ECGs, LBBB, or inability to exercise.
CCTA: High negative predictive value; avoid in high-risk patients likely needing invasive angiography.
2. Medical Management
Prognostic Therapy:
Antiplatelets: ASA 81 mg daily (clopidogrel if ASA-intolerant).
Statins: Per CCS Dyslipidemia Guidelines.
ACEi/ARBs: For hypertension, diabetes, LVEF <40%, or CKD.
Beta-blockers: First-line for angina post-MI or with LV dysfunction.
Symptom Control:
First-line: Beta-blockers or calcium channel blockers (dihydropyridines preferred).
Add-ons: Long-acting nitrates if monotherapy fails.
Avoid: Nondihydropyridines (verapamil/diltiazem) with beta-blockers (risk of bradycardia).
Timeline: Optimize medical therapy within 12–16 weeks before revascularization.
3. Revascularization Considerations
Indications:
Refractory symptoms, high-risk features (Table 5: severe ischemia, LVEF <45%, multivessel disease).
Expedited angiography for high-risk noninvasive findings (e.g., ST depression, ventricular arrhythmias).
Approach:
PCI vs CABG: Decision by multidisciplinary "heart team" (consider diabetes, anatomy, comorbidities).
CCTA: May precede invasive angiography in select cases.
4. Follow-Up & Rehabilitation
Monitoring:
Annual ECG, metabolic labs, and symptom assessment.
Avoid routine stress testing in asymptomatic patients.
Lifestyle:
Cardiac rehab: Referral for all patients, especially post-MI/revascularization.
Exercise: 150+ minutes/week of moderate activity.
Reassessment: For new/worsening symptoms or occupational demands (e.g., commercial drivers).
Key Recommendations
GRADE Strong/High: ASA, statins, ACEi/ARBs in high-risk patients, beta-blockers post-MI.
GRADE Conditional/Moderate: CCTA for LBBB, cardiac rehab referral, no chelation/testosterone.
Take-Home Message:
SIHD management hinges on risk stratification, rapid initiation of guideline-directed medical therapy (GDMT), and judicious revascularization. Prioritize symptom control with beta-blockers/calcium channel blockers, optimize prognostic therapies (ASA, statins, ACEi), and reserve revascularization for high-risk features or refractory symptoms. Regular follow-up and lifestyle modification are critical for long-term outcomes.